University of California, Davis, researchers have developed a new, neuroplasticity-promoting drug closely related to LSD that harnesses the psychedelic’s therapeutic power with reduced hallucinogenic potential.
The research, published in Proceedings of the National Academy of Sciences, highlights the new drug’s potential as a treatment option for conditions like schizophrenia, where psychedelics are not prescribed for safety reasons. The compound also may be useful for treating other neuropsychiatric and neurodegenerative diseases characterized by synaptic loss and brain atrophy.
To design the drug, dubbed JRT, researchers flipped the position of just two atoms in LSD’s molecular structure. The chemical flip reduced JRT’s hallucinogenic potential while maintaining its neurotherapeutic properties, including its ability to spur neuronal growth and repair damaged neuronal connections that are often observed in the brains of those with neuropsychiatric and neurodegenerative diseases.
“Basically, what we did here is a tire rotation,” said corresponding author David E. Olson, director of the Institute for Psychedelics and Neurotherapeutics and a professor of chemistry, and biochemistry and molecular medicine at UC Davis. “By just transposing two atoms in LSD, we significantly improved JRT’s selectivity profile and reduced its hallucinogenic potential.”
JRT exhibited powerful neuroplastic effects and improved measures in mice relevant to the negative and cognitive symptoms of schizophrenia, without exacerbating behaviors and gene expression associated with psychosis.
“No one really wants to give a hallucinogenic molecule like LSD to a patient with schizophrenia,” said Olson, who is also co-founder and chief innovation officer of Delix Therapeutics, a company that aims to bring neuroplastogens to the market. “The development of JRT emphasizes that we can use psychedelics like LSD as starting points to make better medicines. We may be able to create medications that can be used in patient populations where psychedelic use is precluded.”
Testing JRT’s potential
Olson said that it took his team nearly five years to complete the 12-step synthesis process to produce JRT. The molecule was named after Jeremy R. Tuck, a former graduate student in Olson’s laboratory, who was the first to synthesize it and is a co-first author of the study along with Lee E. Dunlap, another former graduate student in Olson’s laboratory.
Following JRT’s successful synthesis, the researchers conducted a battery of cellular and mouse assays that demonstrated the drug’s neuroplastic effects and improved safety profile relative to LSD.
Key findings included:
- JRT and LSD have the exact same molecular weight and overall shape, but distinct pharmacological properties.
- JRT is very potent and highly selective for binding to serotonin receptors, specifically 5-HT2A receptors, the activation of which are key to promoting cortical neuron growth.
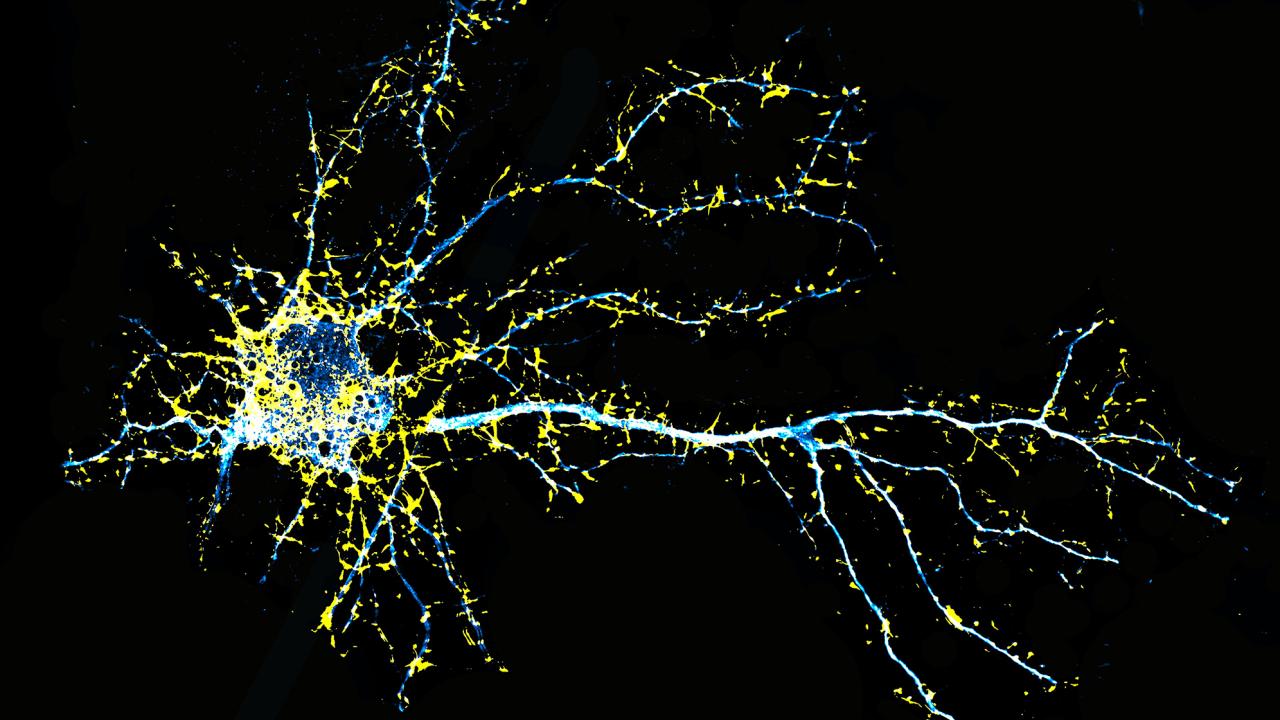
- JRT promoted neuroplasticity, or growth between cellular connections in the brain, leading to a 46% increase in dendritic spine density and an 18% increase in synapse density in the prefrontal cortex.
- JRT did not produce hallucinogenic-like behaviors that are typically seen when mice are dosed with LSD.
- JRT did not promote gene expression associated with schizophrenia. Such gene expression is typically amplified with LSD use.
- JRT produced robust anti-depressant effects, with it being around 100-fold more potent than ketamine, the state-of-the-art fast-acting anti-depressant.
- JRT promoted cognitive flexibility, successfully addressing deficits in reversal learning that are associated with schizophrenia.
“JRT has extremely high therapeutic potential. Right now, we are testing it in other disease models, improving its synthesis, and creating new analogues of JRT that might be even better,” Olson said.
A more effective treatment for schizophrenia
Olson emphasized JRT’s potential for treating the negative and cognitive symptoms of schizophrenia, as most current treatments produce limited effects on anhedonia — the inability to feel pleasure — and cognitive function. Clozapine is the one exception, but it has side effects, and is not first-line drug of choice for people with severe schizophrenia.
Olson and his team are currently testing JRT’s potential against other neurodegenerative and neuropsychiatric diseases.
Additional co-authors include Yara A. Khatib, Cassandra J. Hatzipantelis, Sammy Weiser Novak, Rachel M. Rahn, Alexis R. Davis, Adam Mosswood, Anna M. M. Vernier, Ethan M. Fenton, Isak K. Aarrestad, Robert J. Tombari, Samuel J. Carter, Zachary Deane, Yuning Wang, Arlo Sheridan, Monica A. Gonzalez, Arabo A. Avanes, Noel A. Powell, Milan Chytil, Sharon Engel, James C. Fettinger, Amaya R. Jenkins, William A. Carlezon Jr., Alex S. Nord, Brian D. Kangas, Kurt Rasmussen, Conor Liston and Uri Manor.
The research reported on here was funded by grants from the National Institutes of Health, the UC Davis Provost’s Undergraduate Fellowship, the Camille and Henry Dreyfus Foundation, the Dr. Mohsen Najafi Research Award in Medicinal Chemistry, the Boone Family Foundation, Hope for Depression Research Foundation, the Pritzker Neuropsychiatric Disorders Research Consortium, the L.I.F.E. Foundation, the Chan-Zuckerberg Initiative Imaging Scientist Award, and a National Science Foundation NeuroNex Award.
Media Resources
Molecular Design of a Therapeutic LSD Analogue with Reduced Hallucinogenic Potential (PNAS)
Institute for Psychedelics and Neurotherapeutics
Media Contacts
- David Olson, Institute for Psychedelics and Neurotherapeutics, deolson@ucdavis.edu
- Andy Fell, News and Media Relations, 530-304-8888, ahfell@ucdavis.edu
Greg Watry is an editorial director and content strategist at the UC Davis College of Letters and Science.