When Alyssa Weakley lived 400 miles from her grandmother, the distance and lack of communication brought constant worry and stress. Then 82 and living alone, Janet Dibkey was showing early signs of memory loss.
Dibkey is among the more than 90% of older adults who want to spend their later years in their current home rather than move to an assisted living facility. Weakley is one of the more than 53 million Americans serving as a caregiver to an aging adult or child with special needs. She is also a researcher at UC Davis Health helping older Americans maintain a measure of independence through communication tools and sensor technology.
“You never not worry,” Weakley said. “As a clinical neuropsychologist, I know how cognitive impairment can affect almost every facet of an older adult’s life. I knew there needed to be a solution to improve their life at home while easing the stress on their loved ones.”
A new task management tool
For older adults, mild cognitive impairment and Alzheimer’s disease make it harder to complete important daily activities such as managing medications, paying bills on time and remembering to attend appointments. Weakley designed the Interactive Care Platform, or I-Care, to connect older adults experiencing cognitive impairment to their family members who live apart from them for support in completing these important daily activities.
Created in partnership with older adults with cognitive impairment, caregivers and experts in caregiving, dementia and technology development, I-Care has six main functions:
- a homepage that lists current weather, upcoming events and recent caregiver messages
- a calendar that can be modified by both the care recipient and caregiver
- a to-do list
- a messaging center where care partners can send messages and make video calls
- a collaborative notes section where information regarding doctor appointments and vacation plans can be stored
- a goals section where individuals can track brain health behaviors such as exercise and cognitive engagement
“Not only does I-Care assist with managing everyday activities, but it also addresses social isolation and loneliness in the care receiver and stress and worry in the caregiver,” Weakley explained. “The platform also captures backend data. We hope to use this data to alert individuals when subtle changes occur that may suggest cognitive or health decline.”

California’s aging population
According to the California Master Plan for Aging, the state’s over-60 population is projected to diversify and grow faster than any other age group. That means that by 2030, one-quarter of the state's population will be over the age of 60.
“We are at an inflection point in our communities, with our population aging and becoming more diverse,” said Heather M. Young, co-champion of UC Davis’s Healthy Aging in a Digital World initiative, which has gathered experts to develop technology solutions that enable people to live independently and stay connected to their families and health care teams.
“For the first time in history, we have more grandparents than grandchildren in society. This means families are strained to provide support for their older members, particularly from a distance. We need new creative solutions to support one another.”
As people age, they often share common desires: to remain in their own homes, to maintain their independence for as long as possible, and to rely on family and friends for support when necessary. This concept of staying in your own home as you age is known as "aging in place." However, many older adults and their families have concerns about safety, mobility and daily activities.

Assistive technology supports independent living
Rebecca Boxer, chief of the Division of Geriatrics, Hospice and Palliative Medicine at UC Davis Health, said maintaining independence throughout an older adult’s lifetime can be challenging, especially with multiple chronic conditions or cognitive decline.
“Acute events such as a fall and fracture or the loss of a caregiver can result in a need for increased daily support or institutionalization. Independent living takes community-based or family resources, innovative supportive technologies and a willingness of the older adult to accept assistance when needed,” she explained. “Helping to devise a plan as a person ages for possible eventualities assures that the older adult remains in control of the decisions that would be made for their care.”
An AARP survey showed the many older adults would need to make changes to their home in order to remain safe. Young said that is where technology can help.
“Dr. Weakley’s innovative work is very exciting because she is using technology to support families in ways that are both practical and meaningful. Technology can help organize, coordinate and communicate information that is critical for wellbeing in daily life for both people with dementia and their families,” Young added.

Older adults undergo pilot study testing user-friendliness
Weakley conducted multiple rounds of iterative interface development with experts, individuals with cognitive impairment and caregivers. She then launched a pilot intervention with cognitively impaired individuals and remote caregivers to assess the usability and feasibility of I-Care.
Leeann Patton, who struggles to remember things such as doctor appointments, enrolled in the pilot. The 84-year-old was thrilled when Weakley showed up at her Citrus Heights home with an all-in-one computer with the I-Care software that connected with her sister who lived in Southern California.
“It’s in the dining room area on the table, right out where I can use it with no problem,” Patton explained. “It backs me up where I’ve lost cognition and puts me back in charge of what I’ve forgot.”
Weakley said Patton not only caught on quickly, but soon identified a need Weakley had not thought of — adding a smart watch.
“She would think of something while in her bedroom, but when she walked to the computer, she forgot why she was there. A big gap needed to be solved,” Weakley said.
Patton, who called the system “a reference manual for your mind,” was enthusiastic that her idea would be incorporated into the project.
“It’s just hard to believe! I’m honored so much just to be part of this,” Patton said. “I’m also grateful for the brain God gave me. He must have known I was going to need to do this.”


Importance of technological innovation in senior care
Patton is considered an end user — the person who will use a particular product — of the technology that Weakley is developing. User friendliness is indispensable in any technological endeavor. Because the satisfaction of end users can determine the fate of a new technology, researchers find immense value in collaborating with those who will ultimately utilize it, co-designing solutions to glean valuable insights.
This feedback takes on greater importance as Weakley’s research evolves to include sensor technology. With a network of sensors in one’s home, data can be collected as inhabitants live their lives. In early 2023, Weakley teamed up with Shijia Pan, an engineering professor at UC Merced. Pan has worked on sensors her entire career focusing on how to make them non-intrusive and ubiquitous, but also scalable and reliable.
Pan developed small vibration sensors, roughly the size of a prescription pill bottle. They simply plug into a wall outlet and can fit underneath a nightstand or next to bathroom sink. They essentially map an older adult’s daily routine by recording various vibrations generated by activities such as taking medication or getting out of bed.
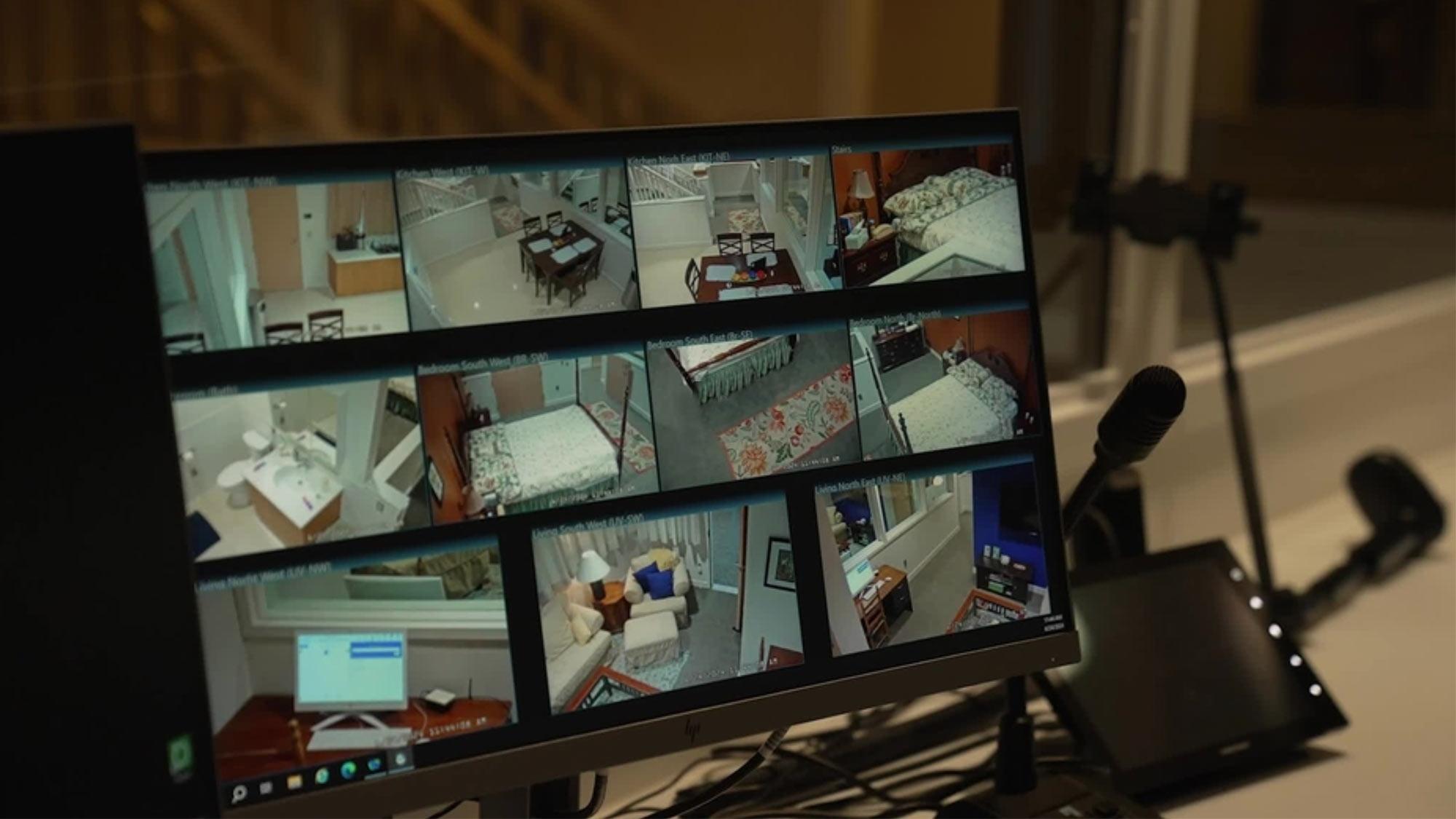
“People touch things all the time, which gives us an opportunity to capture their health data unobtrusively and continuously,” Pan said. “How a person perceives privacy is also very important. If we put something that looks like a camera, people may think their privacy is being intruded, and act differently in the area, and we might not be able to capture their behavior data accurately. I didn’t realize how important that was before I met Dr. Weakley.”

Invisible technology and privacy protection
Pan wants the technology to be as invisible as possible, so that people won’t change their behavior at home. The algorithms they are developing can identify an activity and then visualize the information in the I-Care system so that a remote caregiver can “watch” what’s happening in real time.
“Did my mom get out of bed this morning? Did she take her medicine? Has she fallen? These are the lingering doubts that weigh on caregivers who don’t live in the same home as their family member,” Weakley said.
Because older adults have shared their privacy concerns with Weakley, Pan’s technology allows researchers to monitor activity without revealing sensitive information, such as a phone conversation.
“Instead of directly capturing information a human can understand, the sensors collect information only artificial intelligence can understand,” Pan added.
Making the data understandable by a human user is where UC Davis computer scientist Hao-Chuan Wang comes in. Wang is an expert on human-computer interaction. His visualization interface turns the vibrations into an image that makes sense to users of different roles and needs.
“This data pretty much means nothing [until it is] processed and contextualized to make the information more actionable. We must convert it so that the caregiver knows how to best offer care to the older adult,” Wang said.

Plug-and-play version a goal
Weakley said she hopes to deploy her technology in people’s homes within the next two years.
Her collaborators are aiming for a plug-and-play system that companies want to invest in and people want to use to connect with their families.
“This is just the beginning,” Pan explained. “In the next 10 years, we’ll see the many dramatic changes in the relationship between the human and machine worlds. It’s both a challenge and an opportunity for us to make it a safer world for people who need care.”